What if everything we thought we knew about treating depression was wrong?
What if the phalanx of antidepressants we’ve developed over the past four decades with optimistic names full of X’s and Z’s—Prozac, Zoloft, Paxil—was missing the mark?
What if there was a new treatment that could change our lives? That could enable those of us suffering from depression to stop swallowing that bitter pill every morning? That could undo the ravages not only of depression but of dementia, Alzheimer’s disease and the downhill slide of ordinary aging?
What if there was a drug that all of us might take someday?
I have personal reasons for asking.
Seven years ago I shut down. Amid a crumbling marriage, I became emotionally paralyzed, unable to work, to write, to move. Emails and voice mails piled up unanswered. Slicing an avocado could leave me inexplicably sobbing. Then one day I stopped crying altogether. I went numb. Like so many other depression sufferers, I wondered if death might be easier. The thought scared me.
After five months of seeing a therapist with mixed results, I went to a doctor and walked away with a prescription for 10 milligrams of Lexapro, a cousin to Prozac. I had resisted turning to medication, but it helped. Twenty milligrams helped even more. It didn’t make me feel good, but it made me feel less bad. It was a treatment, not a cure.
Yet a cure may be emerging at an unassuming office building in Rockville just 5 miles from my home.
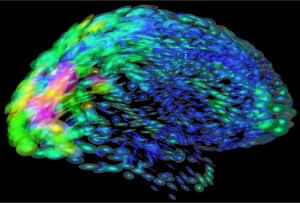
Researchers at Neuralstem Inc. hope to eliminate depression by growing new neurons in the hippocampus, a part of the brain associated with memory and mood, a place deep inside the hemispheres where how we think and how we feel are neurologically entwined. Even the name of the process—neurogenesis—bridges science and the divine.
The company is in the midst of a three-round trial of a drug known as NSI-189. In development since 2000, the compound has shown success in mice, increasing the number of neurons in the hippocampus by as much as 20 percent. Now Neuralstem is conducting the first tests on humans.
“It’s quite revolutionary,” says Paul Currie, a neuroscientist at Reed College in Portland, Ore., who has followed recent scientific strides in understanding neurogenesis, the process by which neurons are generated. Currie cautions, though, that researchers might be moving too fast, and that human trials could be premature. “It’s pretty exciting, but with excitement comes sometimes irresponsibility and overexaggeration, because we’re always looking for that magic bullet,” he says.
Until the ’60s, scientists believed neurogenesis was impossible. The brain was caged inside the skull with no room to grow. Then they discovered that new neurons were being generated inside the hippocampus, possibly to help us process new memories. It was a bright spot in an otherwise grim view of the brain. Cut your finger and it heals. Break your leg and it mends. Even blood refreshes itself. Except for the hippocampus and maybe a few other isolated areas, the brain has a set number of neurons, and they’re dying every day.
“That’s why brain damage and brain diseases are so horrible,” says Richard Garr, the 60-year-old Potomac resident who is Neuralstem’s president and CEO.
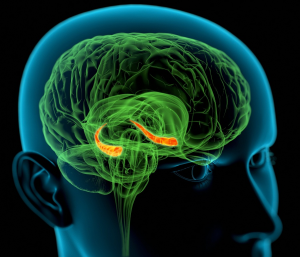
Neuralstem’s gambit is that it can treat not just the symptoms of depression but the very cause by developing a drug that intentionally grows new neurons in the hippocampus. Located deep within the temporal lobe of each hemisphere, the hippocampus takes its name from the scientific designation for the sea horse, which it resembles. Like Alzheimer’s patients, depression sufferers show damage here. A growing body of evidence suggests that antidepressants such as Prozac help repair the damage by creating new brain cells. They do it slowly, though; it’s not what they were designed to do. Neuralstem hopes to speed up the process with a specifically targeted drug.
“People use words like transformative a lot when they shouldn’t,” Garr says. “But if we’re right and it does work, this is completely transformative.”
At a world stem cell conference in London this past May, users of the biotech web platform Total BioPharma placed Garr at No. 15 among the 50 most influential people working on stem cells today. With his short silver hair and narrow face, Garr looks disconcertingly like Roger Sterling, the disaffected ad executive on AMC’s Mad Men. He sits at a tidy desk decorated with models of dissected brains and spinal columns. Tiny, rectangular glasses nearly disappear on his face, and he speaks softly, interrupting his own thoughts by asking, “Right?” to make sure listeners follow along. He is the business side of Neuralstem. Karl Johe, the company’s chief scientific officer, heads up the research end.
A real estate attorney by training, Garr has come to know a lot about how the brain works. Twenty-two years ago, his only son, Matthew, developed a brain tumor. Matthew was just 4 years old, and Garr found himself navigating the complex geography of the human brain and the complications that can result both from a tumor and from the imperfect process of removing it.
Matthew survived, thrived even, but the experience affected him. Now 26, he has trouble remembering, and although he has a driver’s license, he doesn’t feel comfortable behind the wheel. A few years ago he nearly died when fluids that doctors left behind from the removed tumor created complications. They weren’t worried about removing all the fluids, Garr says, because “he wasn’t expected to live this long.”
After a difficult recovery from surgery, Matthew started kindergarten a year late at the McLean School. There he became best friends with a new classmate named Arthur Johe. Meanwhile, Garr became friends with Arthur’s father, Karl, a scientist at the National Institutes of Health in Bethesda.
Karl Johe was pursuing a question tangentially related to Garr’s recent struggles with Matthew’s tumor: He wanted to know how something as simple as a fertilized egg can create something as complicated as the brain.
“I was trying to capture a way to study that moment of switch from being simple to becoming complex,” Johe says. “If we could understand that process, or glimpse into it, then maybe we could learn about how the brain functions.”
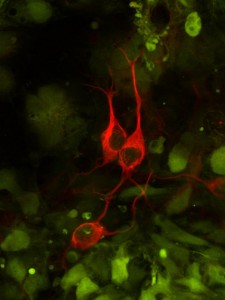
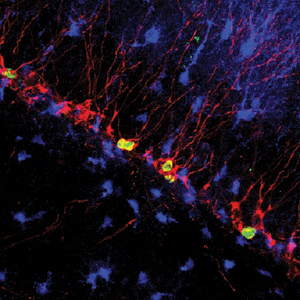
Human embryonic stem cells differentiating into neurons. Neurons derived from embryonic stem cells. National Institute of General Medical Sciences image.
Johe’s question led him to discover neural stem cells. It also unlocked what he hoped could become a treatment for an array of brain disorders. Unlike fetal stem cells, which hold medical promise because scientists can transform them into any cell in the body, neural stem cells only become brain or spinal cord cells. That specialization is their strength, but because they’re also derived from fetuses, they are no less controversial.
“At the time, there was a ban on fetal tissue,” says Johe, now 52 and living in Miami. “At NIH, being the federal government, there was an imminent danger that I could not continue the research.”
Johe was also frustrated by academia and the various agendas of organizations offering research grants. If he wanted to use neural stem cells to find cures, he decided, he needed to form a company.
“Yes, there is a capitalistic motivation,” Johe says, “but the efficiency of achieving the goal is much higher in the private sector. In the private sector, the goal is crystal clear. In an academic setting, that’s not so clear.”
In 1997, the two men partnered to create Neuralstem in a Montgomery County business incubator. Cutting-edge research at NIH and Johns Hopkins University had made the county one of the nation’s top biotech centers. Neuralstem remains there, sharing the building on Great Seneca Highway with GeneImmune, Bethesda Pharma and similar companies.
“Like all parents who are faced with a child’s serious illness, you think about things like research and wonder how you can help, even if it will not help your child,” Garr says. “I felt that this was an opportunity to get involved in a very real way with a technology that could someday be very important for lots of people.”
Sixteen years later, Neuralstem is a “near-virtual” company, with just 16 employees split between Rockville and a San Diego lab. Seven years ago, the company went public with the ambitious stock ticker symbol “CUR.” It’s also leading human trials to treat stroke patients in China, with more planned in countries as far-flung as Mexico and Malaysia.
“We have patients all over the world, and we envision what we call a ‘near simultaneous’ worldwide rollout,” Garr says. The company has secured patents on its compounds worldwide. In many countries, Garr says, trials move faster and cost less than in the United States without sacrificing world-class science.
“How can you not be doing work all over the world?” he asks.
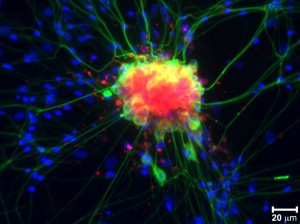
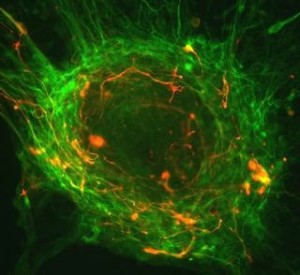
Spinal nerve cells. Neurons derived from embryonic stem cells. National Institute of General Medical Sciences image.
Before its work with the brain, Neuralstem established itself as a leader in repairing spinal column damage. It’s best known for its work in treating Lou Gehrig’s disease. Formally called amyotrophic lateral sclerosis, or ALS, the disease weakens muscle function in the lungs until it suffocates its sufferers. Neuralstem set out to attack ALS by injecting spinal cord stem cells into the spine.
About half of the company’s money and time is still devoted to the creation of its ALS treatment. In 2011, Ted Harada, a former FedEx manager from Atlanta, became a minor celebrity when he made the rounds at CNN and CBS, proclaiming that his disease had receded after he took Neuralstem treatment NSI-566 in Phase I trials.
This past May, the company announced that its drug had virtually halted ALS over the course of two years in six test subjects, including Harada, who has stopped using a walking cane. Last year, Harada was strong enough to take part in a 2½-mile ALS walkathon—a remarkable victory against a disease that can kill in two years. The FDA has approved Phase II trials for the drug at centers in Atlanta and Ann Arbor, Mich., where patients will be given as many as 40 injections of up to 400,000 cells each directly into the spinal column.
The company’s work with depression was serendipitous. Working with neural stem cells meant growing lots of tissue to test various drugs. That process, the company discovered, had other uses.
In the late ’90s, the Clinton administration sought to create a “super soldier” who could stay awake and alert for a week at a time. Neuralstem won a contract to work on the “warfighter of the future” project, Garr says. The company wasn’t focused on creating a drug to keep soldiers awake, however; rather, it was interested in dealing with the consequences of long-term wakefulness. Without sleep, we become irritable, forgetful, irrational—all outward signs of the cell damage that can occur in the sleep-deprived hippocampus.
The Defense Advanced Research Projects Agency (DARPA) eventually canceled the project, Garr says, but Neuralstem moved forward, and NSI-189 was born. If the drug could help sleep-deprived soldiers, as its tests on mice had suggested, then maybe it could help others experiencing cell death in the hippocampus. Maybe it could treat depression, Alzheimer’s, even aging. As we get older, we all lose hippocampal cells. Could this drug make us super seniors?
“Yes,” Johe says. “There’s no question that degeneration of the hippocampus and other parts of the brain is part of the aging process. As we now take many different food supplements to counter or slow that aging process, I see this as a potential ‘vitamin for the brain’ to slow down or counter that aging process in our mental capacity.”
Currie, the Reed College neuroscientist, remains skeptical, however. “The human brain has taken how many millions of years to evolve? I don’t think it’s as simple as, ‘Well, we can improve it,’ ” he says.
Some 27 million Americans like me take antidepressants, according to researchers at Columbia University and the New York State Psychiatric Institute, which published their findings in the Archives of General Psychiatry in 2009. That’s one in 10 people lining up at the movies, driving the Beltway, sampling cheese at the farmers market. More women than men, more whites than African-Americans. And the number is growing.
Is it because depression is being diagnosed more often? Because antidepressants work better than before? Because pharmaceutical companies pressure doctors to prescribe them? Are we more stressed out? More isolated? Are we looking for a quick fix?
Nobody knows for sure, Currie says, but the answer is probably yes to all those questions.
Equally perplexing is why the United States, one of the world’s wealthiest countries, has one of the world’s highest rates of depression. In a 2011 World Health Organization study of 18 countries, only France, land of joie de vivre, had a worse case of the blues, with 21 percent of the population reportedly suffering from depression, compared with 19.2 percent in the United States. South Africa’s rate was half that of the U.S. In Montgomery County, according to a 2009 Centers for Disease Control survey, 16.8 percent of residents reportedly had been diagnosed with a depressive disorder.
Is depression a disease of the privileged? “We just don’t know,” Currie says.
My own depression is relatively mild. I managed to smile and even laugh, so friends and family members didn’t know there was a problem until I told them.
But there definitely was a problem.
A few months into the onset of my depression, I was walking with my dog into a snow-covered field at twilight. The sun had set, and the snow reflected the gray-blue light. Everything around me was a pallid veil. This is what depression looks like, I thought. It felt like I had crawled under a 50-pound blanket and I couldn’t lift it off.
For a while, talk therapy helped, but it didn’t push back the darkness. Mindfulness meditation made it easier to live with, but didn’t lessen it. Medication, however, lifted the veil. I could divorce, remarry, move, start over, get a second chance. Medication was life-changing for me.
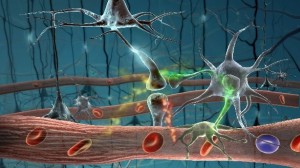
Even leading researchers don’t entirely know why the drugs work, however. We do know that the brain fires impulses from neuron to neuron by way of a number of chemical messengers called neurotransmitters. One of these is a chemical called serotonin. One neuron fires a shot of serotonin across the synapse, the chasm between neurons. The next neuron takes up the message, and the sending neuron recycles the serotonin to do it all again. Prozac and similar drugs called selective serotonin reuptake inhibitors (SSRIs) block that reuptake process, keeping more serotonin at play between the neurons, and apparently boosting the mood-elevating signal.
But what does serotonin do? Unlike other brain chemicals—dopamine, for instance, which we release during sex; or endorphins, which convert pain into pleasure, like a runner’s high—serotonin doesn’t seem to be a happy-making chemical. So why do drugs that keep more serotonin in our brains seem to make us happier?
Recent studies of neurogenesis suggest it may not be antidepressants’ effect on serotonin that makes the difference. Studies on mice have shown that depression symptoms coincide with hippocampal damage. Antidepressants seem to heal that damage. A 2010 Columbia University study found that blocking the healing process prolonged depression, suggesting that without neurogenesis, antidepressants don’t work.
That’s where Neuralstem comes in with its potential wonder drug aimed specifically at rebuilding neurons in the hippocampus.
Like Currie, Lois Winsky, a pharmacology research chief at the National Institute of Mental Health in Bethesda, is reserving judgment of the drug until test results are available and Neuralstem reveals how its stew of organic chemicals works. But she notes that creating new cells isn’t necessarily enough. Those cells have to survive and integrate themselves into circuits that affect mood. It’s not clear if neurogenic drugs can make that happen, she says.
And while dead neurons seem linked to depression, it’s not clear how or why. Losing neurons doesn’t seem to directly cause depression, and more neurons don’t necessarily translate into more happiness. And that’s just in mice, Winsky says. We still don’t know what happens with people.
Even so, other companies are moving in a similar direction, though Neuralstem is the closest to bringing a neurogenic drug to market. Dr. Andrew Pieper, a psychiatrist at the University of Iowa, is also working on a drug to spur neurogenesis. His compound has only been tested on mice, with promising results, but he’s searching for a partner to develop it further. He’s interested in seeing what happens at Neuralstem.
“I really hope their compound works,” he says. “It would fill an important, unmet need for patients. Although some doctors and scientists don’t believe that neurogenesis can be critically involved in depression, we simply won’t know the answer until the hypothesis is tested. I’m eager to see the outcome of their clinical trials.”
Pieper says his compound works by keeping existing cells from dying, allowing more newborn neurons to become integrated into the hippocampus. It also seems to protect cells in other parts of the brain and in the spinal column, possibly offering treatments for Parkinson’s disease and ALS, as well as depression.
“The fact is, the current treatment options for patients with depression simply aren’t good enough,” Pieper says. “Many people are resistant to the effects of the current classes of antidepressant medications available, so we need new treatment options for patients suffering from depression.”
Neurogenic drugs like his or Neuralstem’s may be used alongside antidepressants. Or they may replace them, offering hope to people for whom antidepressants don’t work.
In 2012, 41 patients took Neuralstem’s NSI-189 during a seven-day safety trial. They showed no side effects, Garr says. That paved the way for the Food and Drug Administration to permit further Phase I testing, with 24 otherwise healthy depression sufferers taking increasingly higher doses in three rounds of tests at a center in Glendale, Calif.
In the first round, launched last year, healthy patients were given 40 milligrams a day for four weeks to test the drug’s safety. In the second, patients who were suffering from depression took NSI-189 twice a day. In the final round, due to wrap up this fall, depressed patients take three 40-milligram doses a day.
Throughout each 28-day trial, participants must stay at the center, watching TV or using the exercise facilities to pass the time while researchers monitor their brain activity daily and check their blood, urine and saliva. Researchers give them MRIs when they show up, when they leave, and then four weeks and eight weeks later. It’s a double-blind study. Patients don’t know if they’re taking the drug or a placebo. Researchers won’t know the findings until all three rounds are complete.
If the results look promising and the FDA approves Phase II for NSI-189, Neuralstem will begin stretching the dosing to 90 days and expanding the number of subjects. The company may also launch additional trials involving patients with Alzheimer’s, dementia, traumatic brain injury and degenerative brain diseases.
 Neuralstem is also working with members of the National Football League Alumni Association to develop a trial for treating ex-athletes. There have been a number of high-profile suicides among former players in recent years, some of whom had been diagnosed with traumatic brain injury. Lee Nystrom, a former NFL Alumni Association chairman and ex-Green Bay Packer, says his group is ready to start “pushing the envelope to create therapies” to help ex-players suffering from brain injuries that linger long after they’ve hung up their jerseys.
Neuralstem is also working with members of the National Football League Alumni Association to develop a trial for treating ex-athletes. There have been a number of high-profile suicides among former players in recent years, some of whom had been diagnosed with traumatic brain injury. Lee Nystrom, a former NFL Alumni Association chairman and ex-Green Bay Packer, says his group is ready to start “pushing the envelope to create therapies” to help ex-players suffering from brain injuries that linger long after they’ve hung up their jerseys.
If the results of Neuralstem’s second phase are strong, a third phase would involve hundreds, maybe thousands, of subjects. But even in the best-case scenario, Garr says, it will be five years before someone like me buys NSI-189 at the pharmacy.
Until that time, there are the standard antidepressants.
Over the years, I’ve taken ever-changing drugs and dosages. Ten milligrams of Lexapro, then 20. Forty milligrams of Celexa, Lexapro’s weaker sibling, then down to 20. A year ago I weaned myself off Celexa, chopping the pill into smaller and smaller pieces, and spacing the dosages farther and farther apart until I stopped altogether. I felt good. For a while. Then that familiar feeling returned. Dullness. Darkness. My body so heavy I couldn’t lift it. Thoughts so slow I felt I could grab them out of the air. I made it through six months before I needed to erase the pain.
Now I’m on antidepressants again. Every couple of weeks I grab a handful of pills and subject them to a pill cutter, a little guillotine that slices the pink ovals into two half moons. I take half a day. It’s an act of hope and submission. I still need you, I’m saying, but I only need half of you. One day, maybe, I won’t need you at all.